What are nasal polyps?
Have you ever felt like you have a cold that doesn’t go away? Nasal congestion that doesn’t seem to stop, even with over-the-counter cold or allergy medication, may be due to nasal polyps.
Have you ever felt like you have a cold that doesn’t go away? Nasal congestion that doesn’t seem to stop, even with over-the-counter cold or allergy medication, may be due to nasal polyps.
Picture of nasal polyps
What are the causes of nasal polyps?
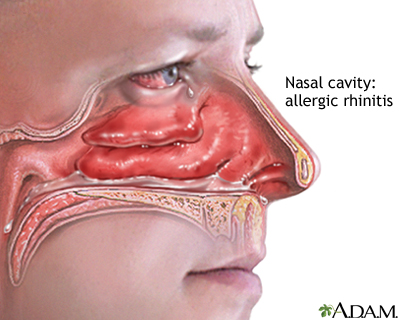
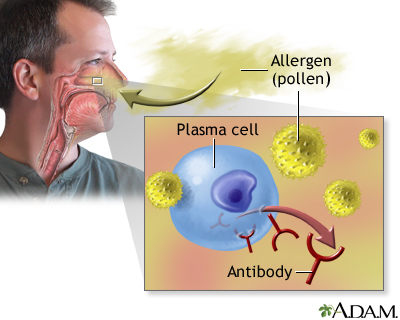
Nasal polyps grow in inflamed tissue of the nasal mucosa. The mucosa is a very wet layer that helps protect the inside of your nose and sinuses and humidifies the air you breathe. During an infection or allergy-induced irritation, the nasal mucosa becomes swollen and red, and it may produce fluid that drips out. With prolonged irritation, the mucosa may form a polyp. A polyp is a round growth (like a small cyst) that can block nasal passages.
Although some people can develop polyps with no previous nasal problems, there’s often a trigger for developing polyps. These triggers include:
- chronic or recurring sinus infections
- asthma
- allergic rhinitis (hay fever)
- cystic fibrosis
- Churg-Strauss syndrome
- sensitivity to nonsteroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen or aspirin
There may be a hereditary tendency for some people to develop polyps. This may be due to the way their genes cause their mucosa to react to inflammation.
Nasal polyps grow in inflamed tissue of the nasal mucosa. The mucosa is a very wet layer that helps protect the inside of your nose and sinuses and humidifies the air you breathe. During an infection or allergy-induced irritation, the nasal mucosa becomes swollen and red, and it may produce fluid that drips out. With prolonged irritation, the mucosa may form a polyp. A polyp is a round growth (like a small cyst) that can block nasal passages.
Although some people can develop polyps with no previous nasal problems, there’s often a trigger for developing polyps. These triggers include:
- chronic or recurring sinus infections
- asthma
- allergic rhinitis (hay fever)
- cystic fibrosis
- Churg-Strauss syndrome
- sensitivity to nonsteroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen or aspirin
There may be a hereditary tendency for some people to develop polyps. This may be due to the way their genes cause their mucosa to react to inflammation.
What are the symptoms of nasal polyps?
Nasal polyps are soft, painless growths inside the nasal passages. They often occur in the area where the upper sinuses drain into your nose (where your eyes, nose, and cheekbones meet). You may not even know that you have polyps because they lack nerve sensation.
Polyps can grow large enough to block your nasal passages, resulting in chronic congestion. Symptoms can include:
- a sensation that your nose is blocked
- runny nose
- postnasal drip, which is when excess mucus runs down the back of your throat
- nasal stuffiness
- nasal congestion
- reduced sense of smell
- breathing through your mouth
- a feeling of pressure in your forehead or face
- sleep apnea
- snoring
Pain or headaches may also occur if there’s a sinus infection in addition to the polyp.
Nasal polyps are soft, painless growths inside the nasal passages. They often occur in the area where the upper sinuses drain into your nose (where your eyes, nose, and cheekbones meet). You may not even know that you have polyps because they lack nerve sensation.
Polyps can grow large enough to block your nasal passages, resulting in chronic congestion. Symptoms can include:
- a sensation that your nose is blocked
- runny nose
- postnasal drip, which is when excess mucus runs down the back of your throat
- nasal stuffiness
- nasal congestion
- reduced sense of smell
- breathing through your mouth
- a feeling of pressure in your forehead or face
- sleep apnea
- snoring
Pain or headaches may also occur if there’s a sinus infection in addition to the polyp.
How are nasal polyps diagnosed?
A nasal polyp will likely be visible if your doctor looks up into your nasal passages with a lighted instrument called an otoscope or nasoscope. If the polyp is deeper in your sinuses, your doctor may need to perform a nasal endoscopy. This procedure involves your doctor guiding a thin, flexible tube with a light and camera at the end into your nasal passages.
A CT scan or MRI scan may be necessary to determine the exact size and location of the polyp. Polyps show up as opaque spots on these scans. Scans can also reveal whether the polyp deformed the bone in the area. This can also rule out other kinds of growths that may be more medically serious, such as structural deformities or cancerous growths.
Allergy tests can help doctors determine the source of persistent nasal inflammation. These tests involve making tiny skin pricks in your skin and depositing the liquid form of a variety of allergens. Your doctor will then see if your immune system reacts to any of the allergens.
If a very young child has nasal polyps, tests for genetic diseases, such as cystic fibrosis, may be necessary.
A nasal polyp will likely be visible if your doctor looks up into your nasal passages with a lighted instrument called an otoscope or nasoscope. If the polyp is deeper in your sinuses, your doctor may need to perform a nasal endoscopy. This procedure involves your doctor guiding a thin, flexible tube with a light and camera at the end into your nasal passages.
A CT scan or MRI scan may be necessary to determine the exact size and location of the polyp. Polyps show up as opaque spots on these scans. Scans can also reveal whether the polyp deformed the bone in the area. This can also rule out other kinds of growths that may be more medically serious, such as structural deformities or cancerous growths.
Allergy tests can help doctors determine the source of persistent nasal inflammation. These tests involve making tiny skin pricks in your skin and depositing the liquid form of a variety of allergens. Your doctor will then see if your immune system reacts to any of the allergens.
If a very young child has nasal polyps, tests for genetic diseases, such as cystic fibrosis, may be necessary.
What treatments are available for nasal polyps?
Medications
Medications that reduce inflammation may help reduce the size of the polyp and relieve symptoms of congestion.
Spraying nasal steroids into the nose can reduce your runny nose and the sensation of blockage by shrinking the polyp. However, if you stop taking them, symptoms may quickly return. Examples of nasal steroids include:
- fluticasone (Flonase, Veramyst)
- budesonide (Rhinocort)
- mometasone (Nasonex)
An oral or injectable steroid, such as prednisone, may be an option if nasal sprays don’t work. These aren’t a long-term solution due to their serious side effects, including fluid retention, increased blood pressure, and elevated pressure in the eyes.
Antihistamines or antibiotics may also treat allergies or sinus infections caused by inflammation in the nose.
Medications that reduce inflammation may help reduce the size of the polyp and relieve symptoms of congestion.
Spraying nasal steroids into the nose can reduce your runny nose and the sensation of blockage by shrinking the polyp. However, if you stop taking them, symptoms may quickly return. Examples of nasal steroids include:
- fluticasone (Flonase, Veramyst)
- budesonide (Rhinocort)
- mometasone (Nasonex)
An oral or injectable steroid, such as prednisone, may be an option if nasal sprays don’t work. These aren’t a long-term solution due to their serious side effects, including fluid retention, increased blood pressure, and elevated pressure in the eyes.
Antihistamines or antibiotics may also treat allergies or sinus infections caused by inflammation in the nose.
Surgery
If your symptoms still aren’t improving, surgery can remove the polyps completely. The type of surgery depends on the size of the polyp. A polypectomy is an outpatient surgery done with a small suction device or a microdebrider that cuts and removes soft tissue, including the mucosa.
For larger polyps, your doctor can perform an endoscopic sinus surgery using a thin, flexible endoscope with a tiny camera and small tools on the end. Your doctor will guide the endoscope into your nostrils, find the polyps or other obstructions, and remove them. Your doctor may also enlarge the openings to your sinus cavities. This type of surgery is an outpatient procedure most of the time.
After surgery, nasal sprays and saline washes can prevent polyps from returning. In general, reducing the inflammation of the nasal passages with nasal sprays, anti-allergy medications, and saline washes can help prevent nasal polyps from developing.
If your symptoms still aren’t improving, surgery can remove the polyps completely. The type of surgery depends on the size of the polyp. A polypectomy is an outpatient surgery done with a small suction device or a microdebrider that cuts and removes soft tissue, including the mucosa.
For larger polyps, your doctor can perform an endoscopic sinus surgery using a thin, flexible endoscope with a tiny camera and small tools on the end. Your doctor will guide the endoscope into your nostrils, find the polyps or other obstructions, and remove them. Your doctor may also enlarge the openings to your sinus cavities. This type of surgery is an outpatient procedure most of the time.
After surgery, nasal sprays and saline washes can prevent polyps from returning. In general, reducing the inflammation of the nasal passages with nasal sprays, anti-allergy medications, and saline washes can help prevent nasal polyps from developing.