Cirrhosis is a late stage of scarring (fibrosis) of the liver caused by many forms of liver diseases and conditions, such as hepatitis and chronic alcoholism. The liver carries out several necessary functions, including detoxifying harmful substances in your body, cleaning your blood and making vital nutrients.
Cirrhosis occurs in response to damage to your liver. Each time your liver is injured, it tries to repair itself. In the process, scar tissue forms. As cirrhosis progresses, more and more scar tissue forms, making it difficult for the liver to function.
Decompensated cirrhosis is the term used to describe the development of specific complications resulting from the changes brought on by cirrhosis. Decompensated cirrhosis is life-threatening.
The liver damage done by cirrhosis generally can't be undone. But if liver cirrhosis is diagnosed early and the cause is treated, further damage can be limited and, rarely, reversed.
Symptoms
Cirrhosis often has no signs or symptoms until liver damage is extensive. When signs and symptoms do occur, they may include:
- Fatigue
- Bleeding easily
- Bruising easily
- Itchy skin
- Yellow discoloration in the skin and eyes (jaundice)
- Fluid accumulation in your abdomen (ascites)
- Loss of appetite
- Nausea
- Swelling in your legs
- Weight loss
- Confusion, drowsiness and slurred speech (hepatic encephalopathy)
- Spiderlike blood vessels on your skin
- Redness in the palms of the hands
- Testicular atrophy in men
- Breast enlargement in men
Causes
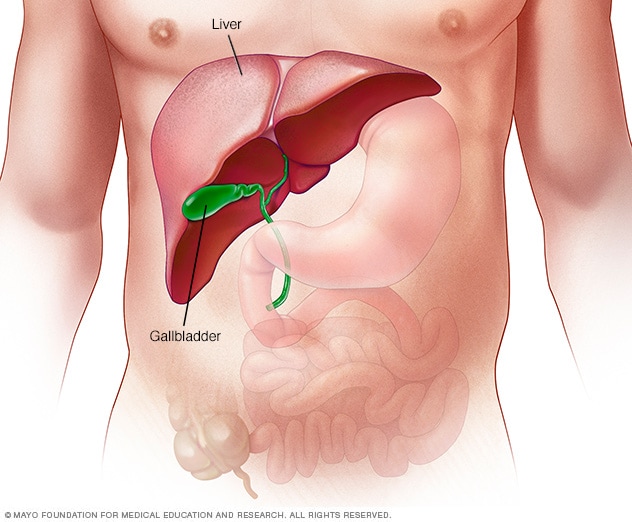
-
The liver
A wide range of diseases and conditions can damage the liver and lead to cirrhosis. The most common causes are:
- Chronic alcohol abuse
- Chronic viral hepatitis (hepatitis B and C)
- Fat accumulating in the liver (nonalcoholic fatty liver disease)
Other possible causes include:
- Iron buildup in the body (hemochromatosis)
- Cystic fibrosis
- Copper accumulated in the liver (Wilson's disease)
- Poorly formed bile ducts (biliary atresia)
- Inherited disorders of sugar metabolism (galactosemia or glycogen storage disease)
- Genetic digestive disorder (Alagille syndrome)
- Liver disease caused by your body's immune system (autoimmune hepatitis)
- Destruction of the bile ducts (primary biliary cirrhosis)
- Hardening and scarring of the bile ducts (primary sclerosing cholangitis)
- Infection such schistosomiasis
- Medications such as methotrexate
Complications
Complications of cirrhosis can include:
Complications related to blood flow:
- High blood pressure in the veins that supply the liver (portal hypertension).Cirrhosis slows the normal flow of blood through the liver, thus increasing pressure in the vein that brings blood from the intestines and spleen to the liver.
- Swelling in the legs and abdomen. Portal hypertension can cause fluid to accumulate in the legs (edema) and in the abdomen (ascites). Edema and ascites also may result from the inability of the liver to make enough of certain blood proteins, such as albumin.
- Enlargement of the spleen (splenomegaly). Portal hypertension can also cause changes to the spleen. Decreased white blood cells and platelets in your blood can be a sign of cirrhosis with portal hypertension.
- Bleeding. Portal hypertension can cause blood to be redirected to smaller veins, causing them to increase in size and become varices. Strained by the extra load, these smaller veins can burst, causing serious bleeding. Life-threatening bleeding most commonly occurs when veins in the lower esophagus (esophageal varices) or stomach (gastric varices) rupture. If the liver can't make enough clotting factors, this also can contribute to continued bleeding. Bacterial infections are a frequent trigger for bleeding.
Diagnosis
People with early-stage cirrhosis of the liver usually don't have symptoms. Often, cirrhosis is first detected through a routine blood test or checkup. Your doctor may order one or more laboratory tests that may suggest a problem with your liver, such as cirrhosis.
Laboratory tests:
- Liver function. Your blood is checked for excess bilirubin, which is a product of red blood cells breaking down, as well as for certain enzymes that may indicate liver damage.
- Kidney function. Your blood is checked for creatinine as kidney function may decline in later stages of cirrhosis (decompensated cirrhosis).
- Tests for hepatitis B and C. Your blood is checked for the hepatitis viruses.
- Clotting. Your international normalized ratio (INR) is checked for your blood's ability to clot.
Your doctor may order imaging and other tests to further diagnose cirrhosis:
- Magnetic resonance elastography or transient elastography. These noninvasive imaging tests detect hardening or stiffening of the liver and may eliminate the need for a liver biopsy.
- Other imaging tests. MRI, CT and ultrasound create images of the liver.
- Biopsy. A tissue sample (biopsy) is not necessarily needed to diagnose cirrhosis. However, your doctor may use it to identify the severity, extent and cause of liver damage.
If you have cirrhosis, your doctor is likely to recommend regular diagnostic tests to monitor for signs of disease progression or complications, especially esophageal varices and liver cancer.
Treatment
Treatment for cirrhosis depends on the cause and extent of your liver damage. The goals of treatment are to slow the progression of scar tissue in the liver and to prevent or treat symptoms and complications of cirrhosis. You may need to be hospitalized if you have severe liver damage.
Treatment for the underlying cause of cirrhosis
In early cirrhosis, it may be possible to minimize damage to the liver by treating the underlying cause. The options include:
- Treatment for alcohol dependency. People with cirrhosis caused by alcohol abuse should stop drinking. If you have cirrhosis, it is essential to stop drinking since any amount of alcohol is toxic to the liver. If stopping alcohol use is difficult, your doctor may recommend a treatment program for alcohol addiction.
- Weight loss. People with cirrhosis caused by nonalcoholic fatty liver disease may become healthier if they lose weight and control their blood sugar levels. It is important to maintain adequate protein intake while attempting weight loss in the setting of cirrhosis.
- Medications to control hepatitis. Medications may limit further damage to liver cells caused by hepatitis B or C through specific treatment of these viruses.
- Medications to control other causes and symptoms of cirrhosis. Medications may slow the progression of certain types of liver cirrhosis. For example, for people with primary biliary cirrhosis (now known as primary biliary cholangitis) that is diagnosed early, medication may significantly delay progression to cirrhosis.
Other medications can relieve certain symptoms, such as itching, fatigue and pain. Nutritional supplements may be prescribed to counter malnutrition associated with cirrhosis and to prevent weak bones (osteoporosis).
Treatment for complications of cirrhosis
Your doctor will work to treat any complications of cirrhosis, including:
- Excess fluid in your body. A low-sodium diet and medication to prevent fluid buildup in the body may help control ascites and swelling. More-severe fluid buildup may require procedures to drain the fluid or other interventions to relieve pressure. At times, a small tube — a transjugular intrahepatic portosystemic shunt (TIPS) — is placed in the vein within the liver to reduce blood pressure in your liver and slow the rate of fluid accumulation.
- Portal hypertension. Certain blood pressure medications may control increased pressure in the veins that supply the liver (portal hypertension) and prevent severe bleeding. Your doctor will perform an upper endoscopy at regular intervals to look for enlarged veins in the esophagus or stomach (varices) that may bleed.If you develop varices, you likely will need medication to reduce the risk of bleeding. If you are not able to tolerate medication and have signs that the varices are bleeding or are likely to bleed, you may need a procedure (band ligation) to stop the bleeding or reduce the risk of further bleeding. In severe cases, a TIPS can be placed in the vein within the liver to reduce blood pressure in your liver and to prevent further bleeding.
- Infections. You may receive antibiotics or other treatments for infections. Your doctor also is likely to recommend vaccinations for influenza, pneumonia and hepatitis.
- Increased liver cancer risk. Your doctor will recommend blood tests and ultrasound exams every six months to look for signs of liver cancer.
- Hepatic encephalopathy. You may be prescribed medications to help prevent the buildup of toxins in your blood due to poor liver function.
Liver transplantation
In advanced cases of cirrhosis, when the liver ceases to function, a liver transplant may be the only treatment option. People usually need to consider this option when they develop symptoms from cirrhosis, such as jaundice, significant fluid retention (ascites), bleeding varices, hepatic encephalopathy, kidney dysfunction, or liver cancer. A liver transplant replaces your liver with a healthy liver from a deceased donor or with part of a liver from a living donor. Cirrhosis is the most common reason for a liver transplant.
Candidates for liver transplant undergo extensive testing to determine whether they are healthy enough to have a good outcome following surgery. Additionally, transplant centers typically require some period of abstinence alcohol for people with alcohol-related liver disease before they can receive transplants






0 comments:
Post a Comment